Diabetes (short, for Diabetes mellitus) is a medical condition whereby there is too much sugar in the blood.
Another condition, Diabetes insipidus, shares a similar name because of the common symptom of frequent urination.
When ‘Diabetes’ is used as a standalone word however, it usually refers to Diabetes mellitus.
This article is in two parts; first, a poem about diabetes, including its symptoms and complications. The second part elaborates on each poem stanza.
Diabetes: the Sugar-Pee Disease
The day is at end, the hour late,
you climb out of bed to urinate;
before dawn, you repeat times eight
Your restless mind begins to debate
what could cause this bladder spate
Weeks later, it’s yet to abate;
by now, it’s like a flood gate
Worried you’ll bed-wet at this rate,
your water, you try to regulate,
but the urge to drink is too great
Time to eat, you fill your plate,
not minding that you just ate
Your raging appetite, nothing can sate,
but one thing you can’t get straight,
you eat and eat, but never gain weight
You start to panic and palpitate,
when ants, on your pee, accumulate
“If it’s too sweet”, you translate,
“then bitter herbs should help negate”;
you forget it’s a family trait
Your condition begins to escalate,
that little boil starts to ulcerate,
blood pressure does not cooperate,
vision appears to deteriorate,
and it’s difficult to concentrate
You call the doctor to pick a date;
after some tests, you get an update,
Insulin is to implicate
The hormone may be inadequate,
or the body’s response, inappropriate
While you tried to self-medicate,
your blood sugar began to appreciate
There may be need to amputate;
your unwitting delay, sealed your fate
Diabetes, you should not underate
'Diabetes: the Sugar-Pee Disease', explained
Background
Blood sugar, Insulin and the Pancreas
Inside the stomach and intestine, acid and ‘digestive enzymes’ break down food into smaller units.
Foods which we classify as carbohydrates, like rice, bread and potatoes become glucose. On the other hand, proteins like meat and fish become amino acids, and oily foods become fatty acids.
Glucose, Amino acids and Fatty acids pass through the walls of the intestines and through the ‘portal vein‘, to the liver.
See ‘The Circulatory System: a look into the Red Prison,’ to learn about ‘the portal vein’ and other blood vessels.
This article focuses mainly on glucose, an important fuel that cells of the body need to function normally.
The liver stores some of the glucose from the diet as glycogen, breaks down some, and releases the rest into the blood.
Another organ, the Pancreas, which lies close to the stomach and liver, releases two hormones, namely Insulin, and Glucagon.
Insulin helps the body cells to take up glucose, while glucagon acts on the liver to release glucose from glycogen stores in response to low blood sugar.
In cases of starvation or fasting for long periods, where there is no glucose from diet and glycogen stores are low, glucagon also helps to promote the breakdown fatty acids or proteins to ‘create’ energy.
The basis of diabetes
Glucose can only enter the cells of the body through specific channels. These channels are known as ‘Glucose Transporters’ (GLUT), and there are 14 types, namely GLUT-1, to GLUT-14.
These ‘glucose transporters’ are distributed round the body, with many cells having more than one GLUT type.
Learn more about the Glucose transporters, here.
GLUT-4 is the only glucose transporter that needs insulin to function. A simple way to look at it is that insulin acts as a key, that opens the GLUT-4 door.
This ‘GLUT-4 door’ is permanently shut and will not open to allow glucose pass into the cells, unless insulin opens it.
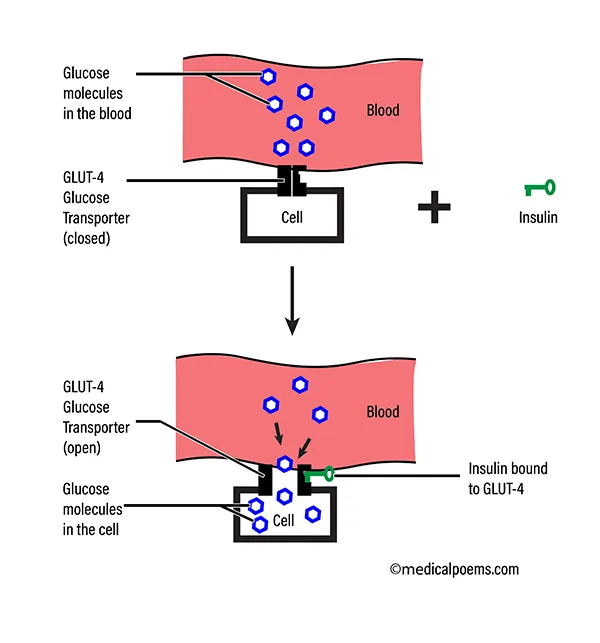
In diabetes, insulin is absent (Type 1 diabetes), not enough, or there is a problem with the way insulin interacts with GLUT-4 (Type-2 diabetes).
Type-1 diabetes occurs when the body’s defense system, that normally fights harmful viruses and bacteria, malfunctions and attacks the cells that produce insulin in the pancreas (autoimmune destruction).
Type-2 diabetes occurs due to a combination of factors like physical inactivity and excessive weight gain. You are also likely to get type 2 diabetes, if a parent or sibling has it (genetic predisposition).
GLUT-4 is present in skeletal muscles (muscles that attach to the skeleton), heart (cardiac) muscles and adipose (fat) tissue.
Stanza 1 (excessive urination, as a symptom of diabetes)
“The day is at end, the hour late, … you climb out of bed to urinate; … before dawn, you repeat times eight … Your restless mind begins to debate … what could cause this bladder spate” (stanza 1, lines 1 to 5)
For many people, excessive urination, also known as polyuria may be the earliest symptom of diabetes.
Of course, there are other conditions that are associated with polyuria, for example, diabetes insipidus, and primary polydipsia.
Normally, all the blood in the body passes through the kidneys, to remove waste via urine. The kidneys maintain a balance of how much water, glucose, electrolytes (like sodium) and so on, is in the blood.
If a particular blood component (except cells) is too much, the kidneys excrete more of it in urine, and withholds it when it is not enough.
In diabetes mellitus, glucose cannot enter the cells, therefore it remains in the blood and its concentration gets too high.
As blood with high glucose levels passes through the kidneys, excess glucose exits the body in urine.
The increasing levels of glucose exiting the kidneys, causes water to follow, a phenomenon known as osmotic diuresis. This means that as the kidneys pass out excess glucose, it also produces excess urine, which is polyuria.
Stanza 2 (excessive thirst, as a symptom of diabetes)
“Weeks later, it’s yet to abate; … by now, it’s like a flood gate … Worried you’ll bed-wet at this rate, … your water, you try to regulate, … but the urge to drink is too great” (stanza 2, lines 1 to 5)
As a continuation of the events in stanza 1 above, increased production of urine leads to increased thirst, known as polydipsia.
Thirst in diabetes, is known as osmometric thirst, as against volumetric thirst, seen in cases like blood-loss, vomiting, or diarrhea.
As the kidneys continually loose water in diabetes, blood volume begins to drop (remember that urine is filtered blood).
Drop in blood volume causes the cells to loose water, to replace that which is lost in urine; consequently, the cells shrink.
Loss of water inside the cells activates the brain to initiate water-seeking behavior, which occurs when you are thirsty.
Increased thirst in diabetes may be limited to a few extra bottles of water a day, or a desperate need to drink any kind of water.
In practice, I have seen someone so thirsty, as to desperately drink from a public rain run-off collection drum. It was a case of Type-1 diabetes.
Stanza 3 (polyphagia, as a symptom of diabetes)
“Time to eat, you fill your plate, … not minding that you just ate … Your raging appetite, nothing can sate, … but one thing you can’t get straight, … you eat and eat, but never gain weight” (stanza 3, lines 1 to 5)
There is a saying that in diabetes mellitus, “cells starve in the midst of plenty”. This is because there is a lot of sugar (glucose) in the blood, up to the point of “wasting” it in urine; however, glucose is unable to get into the cells.
The body senses that the cells are starving, and stimulates appetite, leading to excessive eating, which is polyphagia.
Unfortunately, no matter how frequently one eats, the cells will still keep starving.
In Type-1 diabetes, the absence of insulin causes the breakdown of fatty acids as an alternative source of energy for the ‘starving cells’. Depletion of fatty acid stores means that the fat content of the body drops, which leads to weight loss.
NOTE: Diet aside, the risk of developing Type-2 diabetes increases with body weight, because insulin resistance increases concurrently.
Stanza 4 (other symptoms of diabetes, and its treatment)
“You start to panic and palpitate, … when ants, on your pee, accumulate … “If it’s too sweet”, you translate, … “then bitter herbs should help negate”; … you forget it’s a family trait” (stanza 4, lines 1 to 5)
Asides polyuria, polydipsia and polyphagia, which I discussed above, other symptoms of diabetes include fatigue, general itchiness, and blurred vision.
In up to half of cases, symptoms may be totally absent, that is, asymptomatic. In such cases, the symptoms that patients present with, may point to complications. For example, abdominal pains, nausea and vomiting, and may suggest DKA (Diabetic Keto-Acidosis); see below.
Some individuals report that ants accumulate on their urine, especially in low-resource settings, due to peculiarities of urine disposal. Poor wound healing is also another common presenting symptom in such settings.
The goal of treatment of diabetes is to keep blood sugar level within ‘normal’ range; see stanza 6, below.
Dietary changes, exercise, and weight management, all contribute to better treatment outcomes.
Medications for diabetes include insulin injections and oral glucose-lowering agents, like Metformin and Rosiglitazone.
Keeping the blood sugar levels within normal range helps to prevent complications.
Stanza 5 (complications of diabetes)
“Your condition begins to escalate, … that little boil starts to ulcerate, … blood pressure does not cooperate, … vision appears to deteriorate, … and it’s difficult to concentrate” (stanza 5, lines 1 to 5)
Complications of diabetes usually occur when patients do not take medications according to prescription, typically by skipping doses. On the other hand, medication overdose, also comes with complications
Short term complications
Short-term complications of diabetes usually occur as emergencies. They include:
- Hypoglycemia (low blood sugar): An overdose of insulin, or oral anti-diabetic medications may cause the blood sugar to drop too low. Symptoms include sweating, palpitations and trembling, and in severe cases, seizures, coma and even death.
- DKA (Diabetic Keto-Acidosis): This condition is more common in Type-1 diabetes, whereby absence of insulin causes the body to switch to an alternative energy source, in the form of ketone bodies, from fatty acids. Unfortunately, the acidic ketone bodies accumulate and cause symptoms like nausea, vomiting, acetone breath and abdominal pains; coma and death may follow.
- HHS (Hyperosmolar Hyperglycemic State): This condition occurs more commonly in Type-2 diabetes. Extremely high blood glucose (up to 600mg/dL, or 33mmol/L; see normal range, below) may cause symptoms similar to DKA, but without acetone breath or ketone bodies accumulating.
Long term complications
Complications that may occur over time, include:
- Damage to nerves (neuropathy), which may present as sensory loss (loss of sensation), as well as neuropathic pain (abnormal sensation and pain). Conditions like erectile dysfunction and postural hypotension may also occur.
- Microvascular (tiny blood vessel) damage may affect the retina (diabetic retinopathy), leading to blindness, as well as the kidneys (diabetic nephropathy).
- Macrovascular (large blood vessel) damage, also occur, and may lead to stroke, peripheral artery disease, and coronary artery disease (CAD). CAD is a very common cause of death in people with diabetes.
- Cognitive deficits.
- Diabetic foot ulcers is a common cause of amputations. It usually starts as a little wound that refuses to heal.
- High blood pressure (hypertension) may result from microvascular damage of the kidneys and coronary artery disease. Kidney damage leads to salt and water retention, while stiffening of the blood vessel also increase resistance to flow. Both lead to hypertension; learn more about hypertension here.
- Cataract and Glaucoma.
- Insulin injection site abscess and induration.
Peripheral artery disease and sensory neuropathy make people with diabetes prone to having injuries because they may not feel pain. Poor blood circulation and predisposition to infections also contribute to poor healing.
Stanza 6 (more facts about diabetes)
“You call the doctor to pick a date; … after some tests, you get an update, … Insulin is to implicate … The hormone may be inadequate, … or the body’s response, inappropriate” (stanza 6, lines 1 to 5)
Several ancient texts point to the medical condition which we know today as diabetes. Even now, we still debate some of the facts and nomenclature.
Some experts, for example, still refer to Type 1 diabetes as insulin-dependent diabetes (IDDM), juvenile diabetes or childhood-onset diabetes. On the other hand, non-insulin dependent diabetes, and adult-onset diabetes are terms that point to Type-2 diabetes.
In the midst of all the debate, important facts about diabetes include:
- Over 500 million adults are currently living with diabetes.
- More than 1 million children and adolescents live with Type-1 diabetes
- Almost half of adults living with diabetes do not know.
- Diabetes and its complications cause more than 1 million deaths every year.
- 1 in 6 live births are affected by high blood sugar, in pregnancy.
- Hundreds of billions of dollars are spent every year on diabetes.
A practical method for diagnosis of diabetes, according to the World Health Organization (WHO), is ‘Fasting Plasma Glucose of ≥ 126mg/dL (7.0mmol/L) on two occasions’. Blood for this test is taken in the morning before breakfast, after an overnight fast.
While it is easy to classify diabetes into Types 1 and 2, there is also gestational diabetes which occurs in pregnant women. This type has similarities to type-2 diabetes and the woman is not known to have diabetes prior to the pregnancy. Effects on the baby include high birth weight, heart and physical defects.
Another type of diabetes is Maturity Onset Diabetes of the Young (MODY).
Stanza 7 (final words)
“While you tried to self-medicate, … your blood sugar began to appreciate … There may be need to amputate; … your unwitting delay, sealed your fate … Diabetes, you should not underate” (stanza 7, lines 1 to 5)
The diagnosis of diabetes, can have huge impacts on the life of the patients, as well as family and close friends.
It is mostly a life-long condition, therefore support for the patient is very important, particularly for children who will have to be on insulin.
The following advice may help, as regards better outcomes and quality of life:
- Whether you are on insulin or oral medications, keep a schedule, and don’t skip your medications.
- Try to get an affordable glucometer so that you can monitor your blood sugar at home.
- Learn to recognize the symptoms to low blood sugar (hypoglycemia), like tremors, profuse sweating and dizziness, especially after taking your medications. At the least, always have some candy (sweets) around to quickly mitigate this life-threatening condition.
- Visit an ophthalmologist (a doctor who specializes in treatment of eye conditions), once a year.
- When pregnant, register for antenatal care; in most clinics, you doctor will check, and monitor your blood sugar.
- Ask questions when you visit your doctor, for example, proper technique of using insulin injections to prevent injection-site complications.
- Go for checkups, even when you do not have diabetes, because it usually comes without symptoms.
Conclusion
Diabetes is a medical condition whereby there is too much sugar in the blood, but the sugar is unable to get into the cells.
It occurs when insulin is totally absent or not enough, or the body is not responding normally to the insulin being produced.
Symptoms of diabetes include excessive drinking of water, as well as excessive urination.
Regular checkups and medication compliance is important to prevent complications like retinopathy and nephropathy.




